ORAL SURGERIES

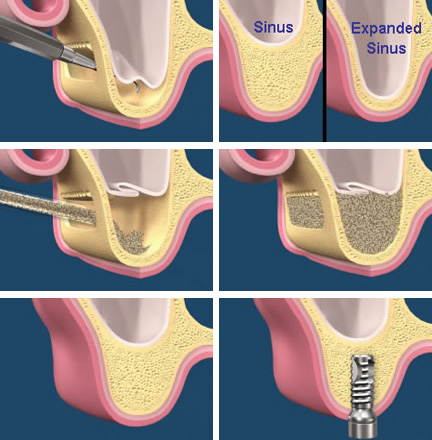
SINUS LIFT
What is the maxillary sinus?
The maxillary jaw bone has two (right and left) cavities, these cavities are usually filled with air and are the largest of the paranasal sinuses. Researchers believe that the paranasal sinuses help reduce the weight of the skull, allow for resonance, and warm inhaled air.
Who needs a sinus lift?
Following tooth extraction, the maxillary sinuses tend to expand into the jaw bone. Sometimes the expansion of the maxillary sinus happens extensively to a degree that prevents implant placement. Dental implants are inserted into bone and when the amount of bone is not enough to hold an implant, a sinus lift is indicated.
How is a sinus lift performed?
There are generally two main methods to performing sinus lifts
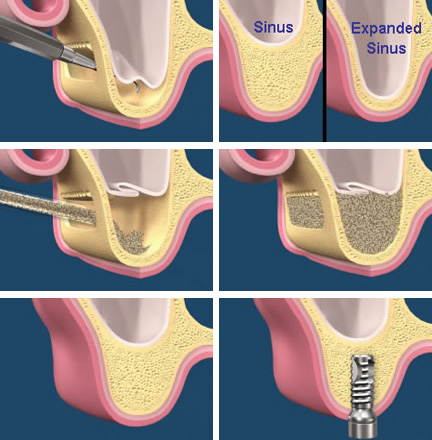
- Internal sinus lift: This is almost always performed at the same time as implant placement, the cavity formed by implant surgery is used to access the floor of the maxillary sinus and help lift it.
- External sinus lift: This is either performed as a separate procedure or concomitantly with implant placement. A separate access is utilized to lift the floor of the sinus cavity and allow for bone grafting.
How would a sinus lift affect my sinuses?
A large number of patients are under the impression that sinus lift procedures are very invasive, and might affect their sinuses significantly. Usually, however, this is not the case. Discomfort in the first few days following surgery are not uncommon, but long term complication are very seldom encountered.
EXTRACTIONS
What is it?
A tooth which is very decayed or damaged, or loose because of gum disease may have to be extracted (taken out of your mouth). Wisdom teeth sometimes have to be extracted if they have come through at an awkward angle and are causing problems (such as decay in adjacent teeth or, being difficult to clean and causing infections). Teeth are sometimes taken out from children’s mouths to help other teeth which are crowded to grow straight, (usually on the advice of an orthodontist).
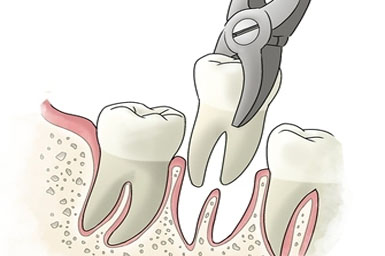
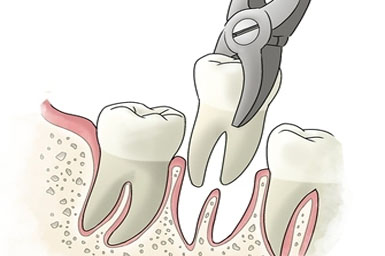
What will my dentist do?
Some teeth are easier to take out than others. A local anaesthetic (an injection in your mouth) will be used to numb the tooth before it is extracted; this is the best treatment for most patients. In some cases, for children or nervous patients, or where a tooth might prove difficult to remove, sedation (something to make you relaxed) with a local anaesthetic may be used, On rare occasions a general anaesthetic may be considered. If a general anaesthetic is needed, you will have to go to a hospital or a specialist treatment centre (you are likely to be able to go home the same day, but not all patients are able to do so).
After working out the best way to take the tooth out, your dentist will discuss with you:
- how to minimise what you feel while the extraction is happening
- whether you should bring someone with you if you are to have sedation or a general anaesthetic
- when it would be convenient for you to have the tooth removed
- you might also discuss other treatment you might need – for example, whether you may require a denture.
While the tooth is being taken out:
You may hear some noise and feel some pressure as the tooth is being eased out — but you should not feel pain. Sometimes stitches are put into the gum to minimise any post extraction bleeding, to make the area more comfortable and help it heal quickly.
Afterwards:
You may need a day or so off work to recover, depending on how difficult the extraction was and whether sedation or a general anaesthetic was used. Most people experience very little post-operation discomfort. The dentist will ensure that bleeding has stopped before you leave the practice. You should not smoke or drink for at least 24 hours after an extraction.
The dentist will give you advice on how to look after the space where the tooth was while it is healing such as:
- which painkillers are suitable to use so you are not in any discomfort when the anaesthetic wears off
- how to contact the practice if there are any problems.
WISDOM TEETH
What are wisdom teeth?
Wisdom teeth are the third molar teeth, also known by dentists as “eights” because of their position in the mouth. They are the last of the permanent teeth to develop.
Why do my wisdom teeth not come up fully?
Because the wisdom teeth are the last to develop and the last to come up (erupt) and because our jaws are often not large enough for all our teeth there is not enough space for them. They may develop in an abnormal alignment.
What does impacted mean?
Impacted means that the tooth is jammed against another tooth or against the jawbone and cannot erupt.
Is this why I can see only part or none of my Wisdom tooth?
Yes. In addition to being deeply situated, they are often covered by a flap or tag of gum, known as the operculum.
Does this cause trouble?
The space between the wisdom tooth and the flap of gum is difficult to clean. Food and other debris known as plaque accumulates and encourages bacterial growth. This may result in several different problems such as inflammation of the gum over or around the wisdom tooth (pericoronitis) which may be quite severe, decay (caries) in the wisdom tooth or in the tooth in front, and gum disease (periodontitis) in the adjacent teeth. Rarely, cysts may develop in relation to buried wisdom teeth.
Removal of wisdom teeth
Removal of wisdom teeth is an operation and like every other operation has side-effects and complications and usually involves the placement of one or more sutures (stitches)


What are the side-effects?
These occur after every operation to some degree. Soreness, swelling and stiffness of the jaw with restricted mouth opening usually clears up after about a week or so after the operation. Some bleeding during the operation is inevitable but this is rarely severe or troublesome.
Does every wisdom tooth removal carry the same risk?
No! It depends on the type and difficulty of the impaction and other factors. The figures below are based on several studies and give some idea of the frequency. Sensory alteration in the tongue: 1:200 (0.5%) Sensory alteration in the lip: 1:250 (0.4%) The decision to proceed with removal of your wisdom tooth (or teeth) can only be made by you. You may discuss it with your family or friends.
What are the complications?
These are much less common but do occur from time to time. Because the nerve to your lip runs through your jaw and the nerve to your tongue lies on your jaw near the wisdom tooth these are at risk of being damaged. This may produce alteration in the feeling in the lip or tongue. This may be felt as numbness (anesthesia) or as “pins and needles” (paraesthesia) it does not involve any paralysis of the lip or tongue. It does not cause any deformity. It can be permanent but this is relatively rare.
Wisdom teeth problems
Complications such as infection, damage to adjacent teeth and the formation of cysts may arise from impacted teeth.
Must all wisdom teeth be removed?
No. Each tooth should be assessed individually and judged on its own merits; other measures are available to control the problem and may be appropriate in your case.
What can I do to help myself?
A mouthwash of medium hot water with a teaspoonful of salt will help to reduce gum soreness and inflammation. (Check that it is not too hot before using it). Swish the solution around the tooth, trying to get it into the areas your toothbrush cannot reach. An antibacterial mouthwash such as Corsodyl can also be very useful to reduce the inflammation. Pain-relieving tablets such as paracetamol or aspirin can also be useful for short-term use, but consult your dentist if the pain continues
Do impacted wisdom teeth cause crooked front teeth?
This is unlikely in most cases and in general unproven but opinion differs about this.
